Arthritis is a term used to describe pain, swelling and stiffness in single or multiple joints.
However, there are many different types of Arthritis. The most common is Osteoarthritis (OA), which affects close to 9 million people in the UK. There are other types of Arthritis, including Rheumatoid Arthritis, which is an inflammatory condition and involves the body’s immune system.
Osteoarthritis (OA) – What is it?
The picture below shows a healthy joint.
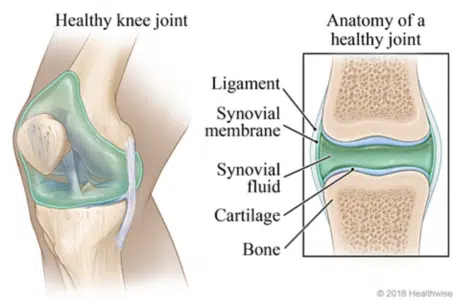
A joint is the part of the body where two or more bones meet to allow movement. Smooth cartilage, which is found on the end of bones, prevents friction as the bones move against one another. In freely movable joints, the entire joint is enclosed inside a membrane filled with a liquid called ‘synovial fluid’ which helps to provide extra cushioning against impact.
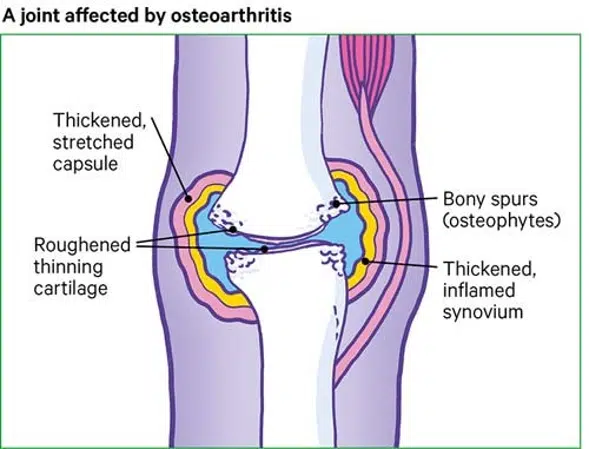
When a joint develops Osteoarthritis, part of the cartilage thins and the surface becomes rougher. This means the joint doesn’t move as smoothly as it should.
When cartilage becomes worn or damaged, all the tissues within the joint become more active than normal as the body tries to repair the damage. These repair processes may change the structure of the joint, but will often allow the joint to work normally and without any pain or stiffness. Meaning that we can have Osteoarthritis in a joint, without having any symptoms at all.
However, the repair processes don’t always work so well and changes to the joint structure can sometimes cause or contribute to symptoms such as pain, swelling or difficulty in moving the joint normally.
For example:
– Extra bone may form at the edge of the joint. These bony growths are called ‘osteophytes’ and can sometimes restrict movement or rub against other tissues. In some joints, especially the finger joints, these may be visible as firm, knobbly swellings.
– The lining of the joint capsule (called the synovium) may thicken and produce more fluid than normal, causing the joint to swell and appear puffy.
– Tissues that surround the joint and help to support it may stretch so that after a time the joint becomes less stable. Muscle de-conditioning due to increased pain levels can also contribute to this.
Another common symptom of OA is ‘cracking’ or ‘grating’ sounds during movement. This is what we call ‘crepitus’. It is likely due to changes to the usually smooth surfaces within the joint or can be from changes in pressure within the joint. It is not a sign that further damage is occurring if heard on its own, although if accompanied by pain may require to be assessed by a healthcare clinician.
It is important to understand that Osteoarthritis is a natural, age-related change. It can be thought of as ‘grey hair for your joints’. Almost all of us will develop Osteoarthritis in some of our joints as we get older, though we may not even be aware of it.
Isn’t OA just ‘wear and tear’ for Old people?
Osteoarthritis usually affects people from the age of 45 onwards and is found to be more common in women than men. The parts of the body most commonly affected by OA are the knees, hips, back and hands (the joints that take the most load or are most active).
OA has often been thought of as ‘wear and tear’, which only affects more elderly people, and is more common in more active people. Through research, we now have a greater understanding of OA. We now know that an individuals chances of developing OA can be affected by several factors such as age, gender, previous injury, weight and genetics.
Further research has shown that we can have an arthritic joint (in some cases with a lot of deterioration) with absolutely NO pain or other symptoms. This has helped us to move on from managing someone’s OA based on a scan and led us to a more person-centred approach to incorporate all of the above factors, along with their symptoms, into their management.
This recent large scale study (link below) showed that knee OA features appeared on scans in up to 43% of asymptomatic (people with no OA symptoms) adults over 40 years old. A great example of how we can have changes in our joints and body but not experience pain because of it.
https://bjsm.bmj.com/content/53/20/1268
How it can affect you?
Like all other health conditions, OA will affect different people in different ways, depending on their situation and symptoms. It may be a pain in the knee that makes climbing the stairs or going for a run more difficult. It may be a reduced range of motion in your shoulder that affects you being able to put on your coat or jumper. It may be a change in the shape of your hand or fingers that prevent you from being able to brush your teeth or open a jar as easily. What we do know is that each person’s condition is different and individual to them.
What brings it on?
Symptoms of OA are usually brought on by changes in physical activity levels. This can be with increased activity levels, such as when a person begins a new exercise like running or swimming. In physio, we often see this in the new year when people take up the gym, or before marathons (like the GNR) when people start training and their activity levels significantly increase from what they are used to. However, OA symptoms can also flare up after periods of inactivity and then return to previous activity levels, this is likely due to de-conditioning of the body’s muscles. At present we are seeing a lot of this due to how Covid has prevented people from doing everything that they were previously.
A common pattern for OA symptoms is that they are worse after periods of prolonged inactivity but then slowly ease with gentle movement, once the joint and surrounding tissues have had a chance to warm up. Other factors such as the weather (hot or cold) or a person’s diet can also impact their symptoms.
Managing ‘flare ups’ is important for people with OA. Flare-ups occur more frequently in a joint with OA than in a joint without. They are usually just a sign that the joint is unhappy or irritated, not that it is more damaged, and often settle down quickly with the right management.
Management of OA:
Although there is no cure for OA at present there are numerous ways in which you can improve the management of your condition and your symptoms.
– Physiotherapy should be your first port of call. We are trained in how to assess your condition helping to identify stiffness, weakness and integrity of the joint or joints involved. Often a look at how the whole system is working will give our clients a better management pathway. Once identified, we then discuss and agree on a rehab management plan that is specific to you.
– Physical activity is a great option that can be used to improve your condition and your overall health. Strengthening exercises can provide more support to a joint and help to offload it by targeting the muscles around it. Mobility exercises can help to decrease the stiffness in a joint. Aerobic exercise can help with the above, as well as maintaining good fitness levels. Exercise also has several other physical and mental benefits so is a great option.
The infographic below, taken from a recent study, shows that running does NOT cause knee OA and that it may even help to prevent it.

Physical activity however can be difficult when you have OA symptoms. If you do too much too soon you run the risk of flaring up your symptoms. A graded, progressive approach to activity is recommended, a prime example of this is the ‘couch to 5K’ running program – start small and progressively increase what you do, as you can manage, and as your body adapts.
– Weight management is important, especially in the weight-bearing joints such as the foot/ankle, knee’s and hips. More weight increases the load going through the joint which can worsen symptoms. A well balanced, structured diet combined with an increase in physical activity is a good starting point if losing weight is your goal.
– Pain relief such as paracetamol or NSAID’s (anti-inflammatories) can be used to ease a person’s pain, making it manageable to move more or exercise. Often people see pain relief as ‘masking the pain’, but when used correctly, can be a brilliant shorter term option to allow better function and help to ease symptoms.
– Steroid injections can be used to try and reduce high levels of pain if previous treatments have not helped, however they are not the first-line treatment.
– Surgery such as joint replacements may be offered when a person’s symptoms are severely affecting their quality of life. It is usually considered after trying other more conservative options, such as those listed above and below.
Other ways to manage:
– Heat/Cold. Heat, such as hot water bottles or wheat packs can be used to relax the muscles which can improve pain and movement. Cold, such as ice packs, can be used to reduce inflammation and can work to reduce pain levels.
– Splints/Supports. You can get splints or braces for the hands/thumb to provide more support or prevent too much movement. For the feet, you may benefit from certain orthotics or footwear. Taping can be a useful support tool to improve feedback and the feeling of security around a joint.
– Massage. Can be used to increase relaxation and decrease stress levels to allow an easier range of movement.
– ‘Pacing & Spacing’. It is important to not stress arthritic joints beyond what they can tolerate. By breaking down larger tasks or adding small breaks in, you will find you can manage a lot more without aggravating your symptoms.
Thanks for Reading
Hopefully, this blog has been useful to you. The main takeaways are that OA is a natural condition that everyone will go through, not something to fear. Occasionally we will get symptoms due to these natural changes, but these can be well managed in various ways that will differ from person to person. Staying active is important in managing and preventing OA.
We are experts in assessing and managing OA so if you have been suffering with symptoms and want a clear plan of how to move forward in the best way for your body, then please get in touch with the clinic.
Written by: Michael Liddle – Senior Physiotherapist